Opioid Epidemic Overview

In September 2017, the White House declared that the opioid drug crisis was a national emergency. This statement came on the heels of the release of a presidential commission report that described the opioid epidemic death rate as ‘September 11th every three weeks.’ After the declaration, the White House instructed federal authorities to use all appropriate power to respond to the opioid crisis.
The White House declaration of an emergency may not have an immediate impact. But it has shone the national spotlight on the opioid epidemic. That bright light can help to solve the problem as more state, local and federal resources are focused on it.
The size and scale of the opioid drug crisis has grown for years to the point that thousands of people are dying from these power drugs each year. This extensive guide has been written to describe the opioid epidemic in detail to give readers a solid grasp of the problem, what is being done, and what the future holds for the opioid problem.
What Are Opioids?
Opioids are mostly prescription drugs that interact with the nervous system to relieve serious pain. Heroin is an illegal opioid. Opioids are all related to one another chemically and affect the opioid receptors on nerve cells found in the brain and body.
Prescribing opioids makes sense in many cases and is perfectly appropriate for certain medical conditions. When they are used properly, opioids such as OxyContin and Vicodin can substantially reduce pain in these types of situations:
- Postoperative pain, such as after abdominal or knee surgery
- Chronic pain due to cancer
- Back pain
- Terminal illnesses
- Osteoarthritis
Prescribing opioids for medically appropriate conditions for a limited period of time by a physician are proper, legal and moral. But when opioids are overprescribed or are taken by people for whom they were not prescribed, a very dangerous situation develops. Addiction comes fast and hard.
Opioids create endorphins in the brain and make people feel good – sometimes 100 times what the body produces. But over time, the drugs cause the brain to stop making endorphins on its own. The only way the person can feel good is by using the opioid.
This fact makes opioids extremely addictive. If their use is not properly supervised by a doctor, the person can become completely hooked on the dangerous drugs. The person may die from them. Overuse of opioids can eventually lead the user to become hooked on heroin. In fact, it is estimated that four in five of heroin addicts started by abusing opioid prescriptions.
And that is how the Opioid Epidemic has developed over the years. Over-prescription of opioids has caused people to become addicted to them and other deadly drugs. The extra drugs from a prescription are sold on the street. The drugs are sometimes modified to be injected or snorted, which leads to an immediate high and increases the likelihood of addiction.
How Bad Is the Opioid Epidemic?
The situation is dire. The Opioid Epidemic is essentially the worst drug crisis in American history. Death rates from opioid overdoses now rival those of AIDS from the 1990s. Overdoses from prescription opioids and heroin (an illegal opioid) now kill more than 30,000 Americans per year.
It’s estimated that between 26.4 million and 36 million people abuse opioids worldwide. (United Nations, World Drug Report). That is equivalent to the entire population of Canada!!
Consider: In 1999, there were twice as many motor vehicle deaths as fatal drug overdoses. By 2014, those numbers were reversed: There were almost 40% more deaths each year from drug overdoses as car crashes. In 2014, 29,230 people died in motor vehicle accidents, and 47,055 died from drug overdoses. In 2015, there were 20,101 overdose deaths due to opioids and 12,990 overdose deaths from heroin.
In 2012, doctors wrote 259 million prescriptions for opioids in the US. This is more than enough to give every adult in the US a bottle of highly addictive pills.
At one time, many of the drug overdoses in the United States were due to cocaine. In 1999, cocaine killed twice as many people as heroin – 3,822 and 1,960 deaths, respectively. By 2014, opioid deaths had skyrocketed 369%, and deaths from heroin had soared 439%.
From 2000-2015, more than 500,000 people in the US died from drug overdoses. It also is estimated that 91 American die each day from an opioid overdose.
It is understood now that the wide availability of prescription opioids available has contributed to the opioid crisis. Major public health efforts are underway to reduce the number of opioid-related overdoses, while still making these drugs available to those who truly need them.
What Is Causing This Epidemic?
Is the opioid epidemic being caused by their prescribed intention or are other factors at play? The question is, what factors? Why are opioids causing the death toll to mount across America, and even across the world? Why has it created so much concern at the highest levels of government, causing the White House to declare it a national emergency in September 2017?
To answer these questions, it is required to possess a foundational understanding of several issues:
The types and uses of opioids nature of addiction, the risks associated with prolonged narcotics use; the epidemic’s beginnings, today’s players, the case against opioids, solutions and what you yourself can do, right now, at home, to protect those you love from being affected. All of these complex factors are covered at length in this article.
- The nature of addiction
- The risks associated with prolonged narcotics use
- The beginning of the Opioid Epidemic
- The stakeholders in the addiction problem
- Potential solutions to the over-prescription problem
- What you can do in your home and community to help.
All of these complex factors are covered at length in this article.
To understand more about the drugs causing the crisis, it is critical to first grasp the different types of opioids and how they are related to opiates.
Opioid Drugs & Prescriptions
The following section lists prescription opioid drugs by brand name.
Opioid Prescriptions by Brand Name
| Abstral | Demerol | Fentora | Nucynta ER | Roxanol-T |
| Actiq | Dilaudid | Hysingla | Onsolis | Sublimaze |
| Avinza | Dolophine | Methadose | Oramorph | Xtampza ER |
| Butrans | Duragesic | Morphabond | Oxaydo | Zohydro ER |
Combination Opioid Prescriptions
These drugs are opioids that are combined with other drugs. For example, Vicodin, Lorcet and Lortab are mixed with acetaminophen to treat moderate to severe pain:
| Anexsia | Lorcet | Percocet | Vicodin |
| Co-Gesic | Lorcet Plus | Percodan | Vicodin ES |
| Embeda | Lortab | Reprexain | Vicodin HP |
| Exalgo | Maxidone | Rezira | Vicoprofen |
| Hycet | MS Contin | Roxicet | Vituz |
| Hycodan | Norco | Targiniq ER | Xartemis XR |
| Hydromet | Opana ER | TussiCaps | Xodol |
| Ibudone | OxyContin | Tussionex | Zolvit |
| Kadian | Oxycet | Tuzistra XR | Zutripro |
| Liquicet | Palladone | Tylenol #3 and #4 | Zydone |
Since there are many different drugs around, people understandably get confused about what are opioids.
The following are NOT opioids:
| Acetaminophen | Exparel | Ketamine | Serotonin/norepinephrine |
| Cocaine | GHS | LSD | |
| Corticosteroids | IV Tylenol | Methamphetamines |
Natural Opiates Vs Synthetic Opioids
It is common to confuse the terms ‘opioid’ and ‘opiate.’ The word ‘opiate’ usually refers to drugs that occur in nature and bind to opioid receptors in the body. Opiates are all made from the opium poppy plant. These include:
- Opium
- Morphine
- Codeine
- Thebaine
Heroin is a semisynthetic drug derived from morphine. It is actually an opioid and not an opiate, but it often referred to as one.
Remember that in a strict technical sense, ‘opiate’ is used to refer to all naturally occurring opiates. ‘Opioid,’ on the other hand, is used in reference to synthetically manufactured drugs that operate similarly to opiates in the human body.
Opiates and opioids work by the same mechanism in the brain and cause the same feelings of euphoria and pain reduction. Thus the line between opiates and opioids can become blurry. Abusers of both opiates and opioids move willingly between one class and another to get a fix, blurring the lines even more. For example, people who once had a legal OxyContin prescription may end up abusing other opioids or opiates they get on the street.
Opiates and opioids are commonly lumped into the same category under the umbrella class “opioids,” and therefore that is the term that will be used throughout this article.
The most common synthetic opioids include these:
- Fentanyl
- Hydrocodone
- Hydromorphone
- Methadone
- Oxycodone
Sources of Opioids
Once the person who was legally prescribed the drug for, say, back pain, is no longer taking the drug, it is possible that they will have pills left over that get into the hands of a non-medical user. After all, there is no low law that says someone who has been prescribed the medication must get rid of extra pills.
The fact is that many people who abuse opioid prescriptions are getting them from friends and relatives, the CDC states according to data obtained from the US National Survey on Drug Use and Health, 2008-2011.
According to the data, 27% obtained the drugs with their own prescription, but 26% got them illegally from a friend or relative for free (CDC – US National Survey, 2008-2011). Twenty-three percent bought them from a friend or relative, and 15% bought them on the street from a drug dealer.
So, a full 64% of those who were abusing the drugs in this survey were not actually prescribed the pills legally! This is a major driver of the Opioid Epidemic. Any solutions to the problem must address this fact specifically.
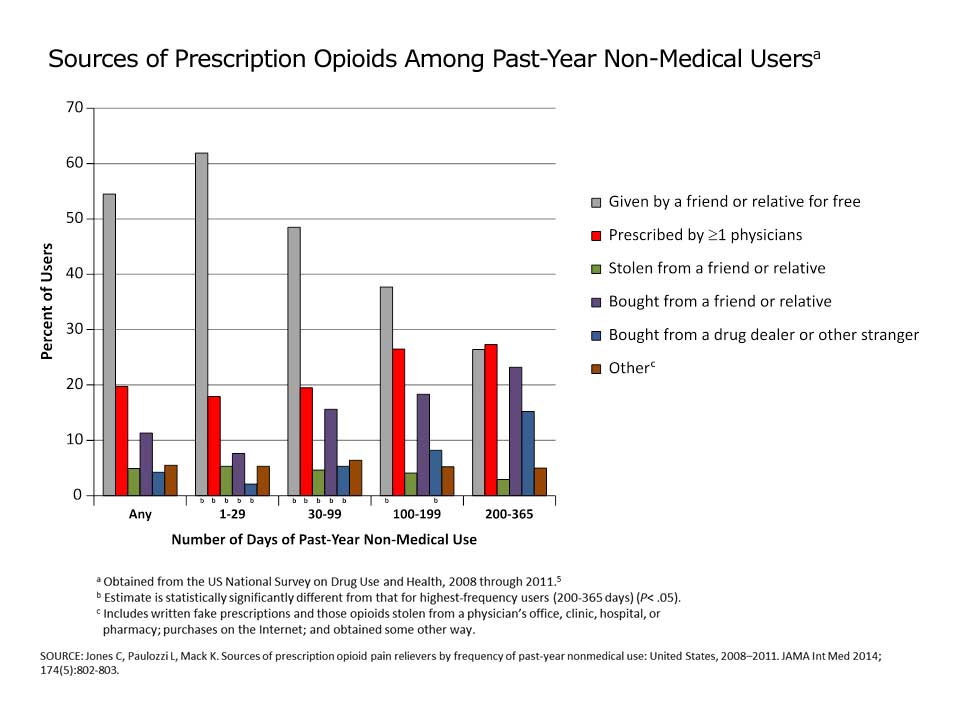
The survey also shows those at highest risk for overdose are 400% more likely than average to buy drugs from a dealer. Also, approximately 4-5% of those in the data were shown to have stolen the pills. The problem also is being exacerbated by doctors who continue to prescribe the drugs to patients after 100 or even 200 days. But it has been shown if you are on opioids for more than 90 days, your risk of becoming addicted increases 15-fold.
Fentanyl is particularly problematic for addiction because it is 50 times more powerful than morphine. Overdose deaths from Fentanyl in 2016 are up 540% in three years! (National Center for Health Statistics, Centers for Disease Control and Prevention)
It doesn’t help that fentanyl can be illicitly manufactured, and street versions are even more dangerous than their federally approved counterparts. The data generally point to a fundamental aspect of this crisis: Many who are prescribed opiates and opioids are not the ones forming the addiction. Rather, it is the people around them, who have access to their pill drawers and medicine cabinets, who are forming addictions, suffering and dying.
The facts paint a frightening picture, one stark enough to alarm anyone who has to bring opioids into their home due to pain, surgery or cancer-related palliative care. The dangers to loved ones and others with ready access to the medicine cabinet are all too obvious.
Opioid Epidemic Statistics
To get a handle on the devastating impact that opioid addiction is having on America, we need to dive deeply into the statistics. The numbers are ugly and growing uglier.
For example, more than 50,000 people in the US died from drug overdoses in 2015, the most ever, according to the CDC. This grim milestone was reached in part due to the soaring problem of opioid addiction. Heroin, which is an illegal opioid, saw a 23% rise in deaths in a year to 12,989 (Chicago Tribune). This is a bit higher than the number of gun homicides for that same year.
It is expected that drug overdose deaths for 2016 will be in the range of 59,000, although that data is not in yet.
Deaths from synthetic opioids such as fentanyl, spiked 73% to 9580 in 2015. Prescription painkillers such as OxyContin and Vicodin killed 17,536, which was a 4% increase.
According to Robert Anderson, who manages death statistics at the CDC, the country has never seen a crisis quite like the Opioid Epidemic, at least in modern times. Anderson’s department reported that overall drug overdose deaths increased to 52,404 in 2015, which was an 11% increase. This was substantially higher than the number of people who died in auto accidents – 37,757. Gun deaths, which included suicides and homicides, rose 7% to 36,252.
The data shows that more people are dying in America from drug overdoses than car accidents and shootings. This is indeed a national crisis. (Robert Anderson, CDC)
CDC also noted that the nation’s life expectancy in 2015 declined for the first time in more than two decades. Drug overdoses were a significant factor in this fact. There are many other alarming opioid epidemic statistics to consider as we try to wrap our arms around this crisis.
The following list highlights some of the most alarming statistics today:
- Drug overdoses are now the leading cause of death among Americans under 50; it is the leading cause of accidental deaths for all Americans.
- Opioid misuse alone costs the United States $78.5 billion a year.
- Sales of prescription opioids in the US increased by 400% from 1999 to 2014.
- Fentanyl (an opioid) is 50 times more powerful than morphine.
- Fentanyl deaths in 2016 are up 540% in three years.
- Over 43,000 Americans die each year due to overdose, 187,000 globally.
- America makes up 5% of the world’s population but consumes 80% of opioid medication.
- Drug overdose deaths in 2016 most likely exceeded 59,000, the largest annual jump ever recorded in the United States.
- In 2015, 276,000 teenagers were using pain relievers for nonmedical uses. It was estimated that 122,000 were addicted to prescription painkillers.
- In 2016, 212 million opioid prescriptions were written. This is more than enough to give every adult in America their own bottle of pills.
- Four out of five new heroin users started their drug problem by abusing prescription painkillers.
- More than 90 Americans die from opioid overdoses every single day.
- Estimated that between 26.4 million and 36 million people abuse opioids worldwide.
- Every day, 142 people in the U.S. die from overdoses of legal opioids.
Additional Statistics
- 70% of healthcare practitioners believe opioid addiction is treatable, while only 47% of the American public does. (Cigna Study)
- In 2015, nearly 80% of the 2 million Americans suffering from opioid addiction did not receive treatment. (Cigna Study)
- 47% of medical practitioners state addiction usually develops after a necessary prescription for pain management. (Kaiser Family Foundation)
- 40% of the general public has either experienced opioid addiction or knows someone who has. (Kaiser Family Foundation)
- US deaths due to opioid overdoses in 2015 varied by age: 3165 for those 24 and younger; 8568 for those 25-34; 7484 for those 35-44; 7595 for those 45-54; and 6277 for those 55 and older.
- Overdoses are more likely among non-Hispanic whites and American Indians or Alaskan natives than among non-Hispanic blacks and Hispanics. (Cigna Study)
- The top five states in opioid-related overdose deaths in 2015 per 100,000 of population were West Virginia – 36; New Hampshire – 31.3; Ohio – 24.7; Massachusetts – 23.3 and Kentucky – 21. (Cigna Study)
Below is a chart from the CDC that shows the number of drug deaths in the US and how they are rising.
CDC’s standard analysis approach as seen below has combined the natural, semi-synthetic, and synthetic opioid categories (including methadone) when reporting deaths involving opioid analgesics, also referred to as prescription opioids. Using this method, in 2015 there were over 22,000 deaths involving prescription opioids, equivalent to about 62 deaths per day. This is an increase from approximately 19,000 in 2014.1
Economic Burden of Opioids
We know that the opioid epidemic has caused a major public health crisis, and we know that it kills thousands of people each year. But the crisis also has a very damaging effect on the US job market and economy.
The abuse of opioids is a major factor in why many prime age, male workers are unwilling or unable to find a job, according to a recent Goldman Sachs report. Economist David Mericle stated in the report: “The opioid epidemic is intertwined with the story of declining prime-age participation, especially for men. The crisis has created significant costs both to employers and the public sector.”
This has caused the US labor force to shrink, which tends to reduce wage and economic growth for the country. Both wages and economic growth have been tepid since the Great Recession.
As of 2017, the labor participation rate for men 25-54 has fallen by 10% since the peak in the 1950s. Currently, it stands at 88.4%, which is a bit higher than the all-time low in 2014 of 87.9%.
Approximately 1.8 million workers are reported to be out of the labor force for ‘other’ reasons. This means that they are not retired, in college, disabled or caring for a loved one. Of those people, it is estimated that approximately 881,000 of them have taken opioids recently.
Also, the Centers for Disease Control and Prevention estimates that the total ‘economic burden’ of prescription opioid misuse alone in the United States is $78.5 billion a year, including the costs of healthcare, lost productivity, addiction treatment, and criminal justice involvement. This represents a huge increase in the problem.
According to a report published by the Centers for Disease Control, “Since 2000, the rate of deaths from drug overdoses has increased 137%, including a 200% increase in the rate of overdose deaths involving opioids (opioid pain relievers and heroin)” (Rudd, 2016).
The report adds that these increases are somewhat agnostic, affecting huge swaths of the American population: “The rate of drug overdose deaths increased significantly for both sexes, persons aged 25–44 years and ≥55 years, non-Hispanic whites and non-Hispanic blacks, and in the Northeastern, Midwestern, and Southern regions of the United States.” In 2015, according to the National Institute on Drug Abuse, this number jumped to 33,000 deaths (2017).
Opioids Effect on Women and Children
There was a time when the people who abused opiates were mostly men. In the 1960s when heroin first hit the scene, more than 80% of junkies abusing the drug were men. But times have changed greatly.
With the introduction of opioids a few decades ago, the number of women who abuse both opiates and opioids has risen dramatically. One estimate is that 46.4% of abusers of opiates and opioids are women.
Women can be more likely to become hooked on opioids than men for some unusual reasons. Women are more likely to go to the doctor to fix whatever health problem they have. Men tend to not visit the doctor as often. The doctor might listen to the woman’s complaint about monthly cramps or a backache and prescribe an opioid to take care of the problem. Women also are more likely to get a prescription for a higher dose of opioids and for longer times than men.
Biologically, there also are factors in play with women to make the epidemic affect them differently. Women have a higher amount of body fat and a lower amount of water. Their bodies absorb and metabolize drugs differently than men’s do. During their period, they feel less of an effect from the drugs they take, so they might take more during that week. This can cause an upward spiral in a number of opioids they take.
Women also are more sensitive to feelings of anxiety and depression than men and may seek out opioids or opiates to deal with them.
Further, women may become dependent on prescription pain relievers more quickly than men,” says the American Society for Addiction Medicine, or ASAM (2016). Illustrating this is the fact that “Prescription pain reliever overdose deaths among women increased more than 400% from 1999 to 2010, compared to 237% among men,” the same source explains.
There is one bright side, however: Women seem to absorb what they learn in drug rehabilitation and treatment better than men. It may take them awhile to get treatment, but they tend to make good progress once they are there.
Opioids Effect on Children
The opioid epidemic has devastating effects on the most vulnerable among us, especially children. Many children are seriously affected by the problem through their parents’ addiction, and/or through their own. It is estimated that at least 2 million children are exposed every year to parents who use illegal drugs, including opioids.
This is significant because parents’ abuse of opioids is a major health and safety risk for children. For example, infants whose mothers used drugs during pregnancy are much more likely to have serious mental, physical and behavioral problems. One of these issues is called neonatal abstinence syndrome or NAS. This is a post-birth withdrawal syndrome that is usually caused by prenatal exposure to opioids.
NAS symptoms in babies include tremors, crying excessively, poor eating which leads to health problems, and rapid breathing. The incidence of NAS has risen by 300% from 1999 to 2013.
Substance abuse also leads to poor and inconsistent parenting. This, in turn, leads to children not having their basic needs met: nutrition, supervision and nurturing.
Another problem is that children who have parents with drug problems are much more likely to be abused and neglected. This leads to more of these children going into the child welfare system. Children also can become hooked on opioids themselves if they prescribed them inappropriately. Adolescents and young adults are also particularly at risk, both because they often get prescription pain relievers for free from friends and relatives, and because they are prescribed them so much more often.
The numbers spiked between 1994 and 2007 (ASAM, 2016). And in 2015, “276,000 adolescents were current nonmedical users of pain reliever, with 122,000 having an addiction to prescription pain relievers.”
To keep opioids out of the hands of children, experts in the field recommend that teens be educated about the perils of opioid use. They also recommend that when doctors prescribe them to children, they issue the minimum number of pills so that there is none left over.
Opioids Effect on the Workforce
Some labor and economic experts maintain that the opioid epidemic has had a substantial, negative effort on the American workforce participation rate.
It is believed that this effect has been particularly pronounced in the critical demographic of 25-54-year-old men, reports Princeton University Professor of Economics Alan Krueger.
The professor noted in a September 2017 Bloomberg interview the following points about the opioid crisis and workforce participation:
- The US is 5% of world population and we are prescribed 80% of opioids. Krueger believes over-prescription of opioids is a factor.
- Men who are between 25-54 report a higher level of pain, which can lead to a lower rate of workforce participation.
- People who are taking opioids to manage pain may have difficulty passing work drug tests.
- 47% of men not in the labor force are taking some type of pain medication, and 20% of that number is prescription drugs.
- Labor force participation rate for 25-54 has fallen by 3% in the last 15 years.
- Krueger believes that 6/10s of 1% of that 3% are due to the spread of opioid medication abuse. About 20% of the decline for men is due to the opioid crisis, he believes.
Krueger also noted in the interview that some parts of the US report a very high number of opioid prescriptions. For example, in the southwestern Virginia town of Norton, there are over five opioid prescriptions per person. This is far beyond a normal level, which he believes could be due to doctors prescribing much more opioids than medically necessary.
Opioid Effect on Veterans
Treating veterans with opioid addiction is more challenging than treating other sufferers. This is because many veterans who return from overseas deployments suffer from chronic pain, PTSD and other ailments that require medical intervention. One-third of medical practitioners reported in a recent survey by the Economist Intelligence Unit (EIU) that they are not highly confident that they have adequate training and resources to treat veterans with addiction problems.
The EIU survey revealed that veterans were more focused on chronic pain issues than other Americans and the need to treat it effectively. According to the survey:
- 53% of veterans stated that addiction usually develops after a necessary prescription to manage pain; this compares to 47% of the general public who said the same.
- 40% of veterans stated that opioid addiction develops among those who suffer pain, such as veterans and athletes, while 35% of the general public said the same.
The survey further showed that many military veterans have ideas of the types of treatments that could help them.
- Veterans stated 32% of the time that the medical community should provide less addictive painkillers to reduce the opioid supply in the public; this compares to 26% of the public who had the same view.
Veterans also stated more often than the general public (38% to 31%) that they wanted to expand access to medical treatment with both traditional and alternative practices in their community.
Caregivers for veterans also reported in this survey that they wanted to be better trained on how to recognize addiction signs in their veteran patients.
Other statistics involving veteran opioid use reveal the extent of the problem:
- From 2010 to 2015, the number of veterans with opioid addiction climbed to 68,000, which is a 55% increase in that period.
- Those veterans living with an addiction to opioids make up 13% of all veterans being prescribed the drugs.
- There was a 52.7% increase in veteran outpatients who were treated for various substance abuse disorders from 1995-2013.
- 75% of healthcare practitioners think that treating veterans with opioid addiction is more complicated than treating other patients; they believe that issues such as PTSD and chronic pain are major factors.
- The VA reports that 60% of returning military veterans who were deployed in the Middle East and 50% of veterans from earlier deployments had problems with chronic pain. That compares to 30% of the general public who deals with chronic pain.
Solving the Opioid Epidemic will involve considerable effort addressing the unique needs of our military veteran community. Special efforts will need to be made by stakeholders to ensure that veterans with chronic pain get the relief they need, while also ensuring that that relief does not spiral downward into addiction.
Opioid Prescription Rates
Sales of prescription opioids in the US increased by 400% from 1999 to 2014, according to the CDC. However, there has not been a corresponding increase in the amount of pain that people in America report. During this time frame, the number of prescription opioid deaths rose in a similar fashion.
Data published by the CDC finds that approximately one out of five patients with pain not related to cancer or another pain-related diagnosis are prescribed opioids. From 2007 to 2012, the rate of specialists prescribing opioids for pain rose significantly. This has led to a corresponding increase in abuse and dependence of the drugs.
Sales of prescription opioids in the US increased by 400% from 1999 to 2014, according to the CDC.
Healthcare providers have reported to CDC widespread concern about the risk of opioid addiction and overdose. Some doctors also have reported they lack sufficient training to manage pain for patients, which can lead to overprescribing. The CDC reports that prescription opioids may not be appropriate for improving chronic pain and function.
The rising number of people prescribed opioids also has led to the illegal use of opioids. The CDC reports that many people who abuse opioids get them for free from a friend’s or relative’s prescription. Some people also sell their prescribed pills to friends, relatives or on the street.
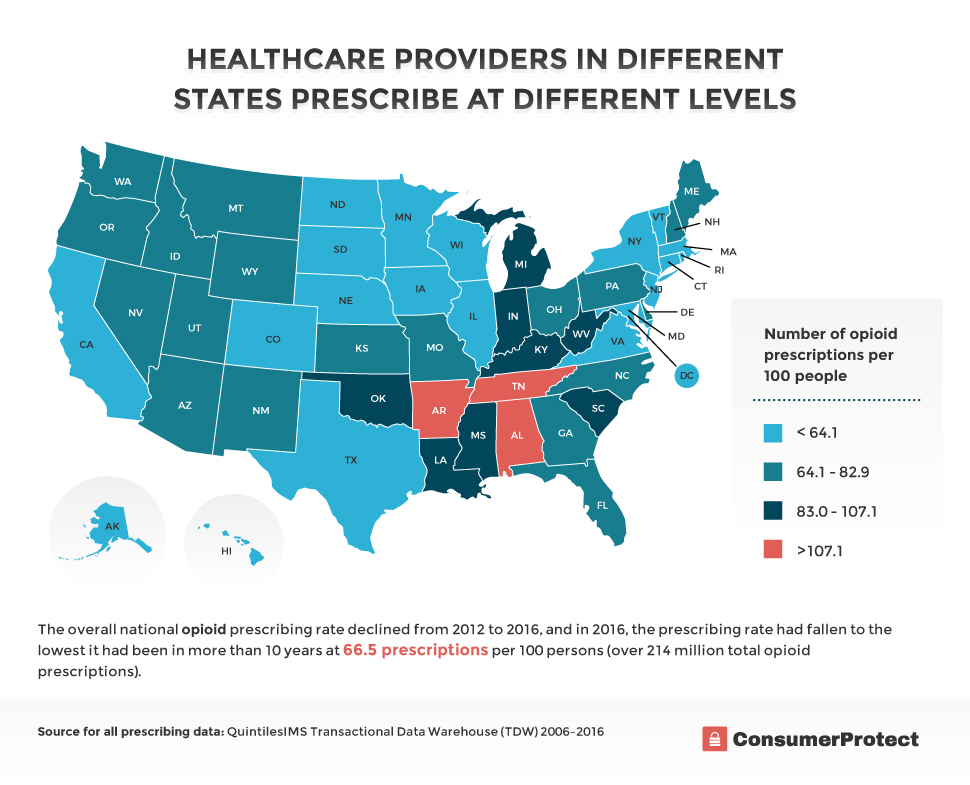
A number of opioid prescriptions given vary widely by state. 2016 data from CDC reveals that healthcare providers in states with the highest rate of prescriptions wrote almost three times as many prescriptions per person as those in the lowest level states. Health issues that cause substantial pain do not vary that widely from place to place. Therefore, there must be other explanations for the variability, such as overprescribing.
The data in this map shows the geographic distribution in the United States at the state level of retail opioid prescriptions dispensed per 100 persons in 2016:
The Shape of Addiction
Addiction is a tough definition to pin down. Many definitions exist as there are publications to voice them. According to ASAM, for instance, “Addiction is a primary, chronic and relapsing brain disease characterized by an individual pathologically pursuing reward and/or relief by substance use and other behaviors” (2016).
Addiction is also often characterized by the effects it has on the life of the user. Explains the National Center on Addiction and Drug Abuse: “Addiction is a complex disease, often chronic in nature, which affects the functioning of the brain and body …the most common symptoms of addiction are severe loss of control, continued use despite serious consequences, preoccupation with using, failed attempts to quit, tolerance and withdrawal” (2017).
However you define addiction precisely, the US has been leading in opioid addiction and consumption for a long time, say Lyapustina and Alexander. “The United States has been at the forefront in terms of prescription opioid consumption. In 2009, the United States consumed 99% of the world’s hydrocodone, 60% of the world’s hydromorphone, and 81% of the world’s oxycodone” (2015).
Prescriptions of opioids soared in the 1990s and 2000s as pharmaceutical companies were hard at work campaigning that these drugs are safe. This was despite evidence from the early 20th century that the drugs were highly addictive and inherently not safe.
Concurrently, politicians were approving lobbyist goals and regulators passed new pills along with accelerating regularity. It wasn’t until people began dying by the thousands that governments started paying attention. Few are demanding an outright opioid ban, as there are legitimate medical uses for powerful painkillers. But experts across the board have noted the reckless way in which the medical community began prescribing these medications in response to pharmaceutical industry reassurance.
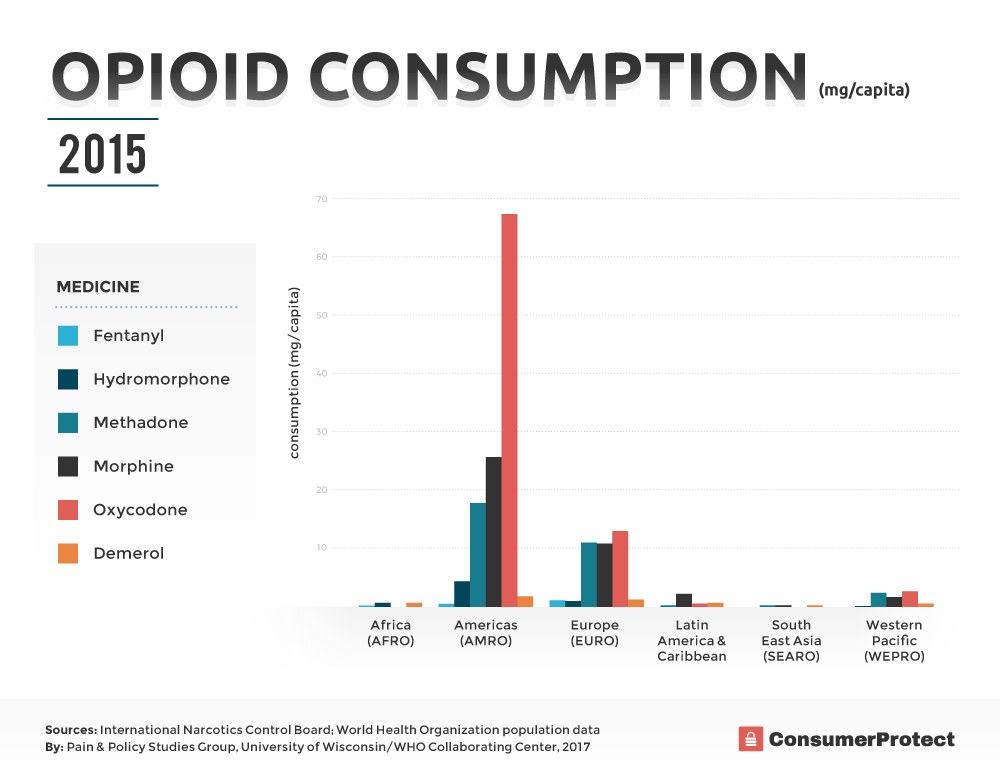
The following chart shows total consumption by country for 2015 (the latest data available) as reported annually to the International Narcotics Control Board. The Americas by far have the highest level of opioid consumption, with oxycodone being the most common opioid prescribed. Such high levels of opioid prescription has led to a serious opioid dependence problem, and solutions are desperately needed.
What Is Opioid Dependence?
Opioid dependence is when a person is both psychologically and physiologically addicted to opioids. The typical addict will continue to use the drug even though it is causing serious personal, social and physical problems. Many patients become dependent upon opioids after being prescribed them for postoperative pain. Symptoms of addiction to opioids include chills, tremors, sweating, itching, anxiety, nausea, and depression.
Common results of opioid dependence include:
- Loss of employment
- Broken relationships with friends and family
- Loss of sleep and appetite
- Change in morals (such as resorting to theft)
- Disinterest in engaging in normal activities
- Withdrawing from social activities and scenes
- Over- and underactivity
- Inability to quit, despite repeated efforts
- Depression and anxiety
- Paranoia
- Dark or suicidal thoughts
Over time, these largely psychological effects transition to very serious medical conditions. Though that is not to downplay the significance of suicidal ideation by any means, it is important to recognize that even for those who don’t experience such feelings, the consequences can be extremely dire. According to Eric Patterson (2017), they include:
- Respiratory distress
- Nausea and stomach upset
- Constipation and inability to have a bowel movement
- Abdominal bloating
- Liver damage
- Neonatal problems, which can lead to serious birth defects
- Lack oxygen to the brain (from respiratory depression)
Being addicted to opioids has many terrible personal, professional and physical consequences. How does this happen?
Causes of Opioid Addiction
Opioids, like all other drugs, work by affixing themselves to preexisting receptors in the nerve cells of the brain, spinal cord, and nervous system. These receptors are there to enable the body to do things such as calm nerves, relieve depression and reduce sensations of pain. In a drug-free human body, the molecules that attach to them are naturally occurring, or “endogenous,” such as endorphins.
These naturally occurring opioids are normal and non-addictive, which means no matter how many endorphins you create – from exercising, eating desserts you love, having sex, and other pleasurable activities – you cannot get addicted to them. It’s natural for your brain to find these activities rewarding because your body benefits from them and it is therefore evolutionarily advantageous for you to like them.
Endorphins, however, aren’t the only chemicals that may attach to these receptors. Both naturally occurring and synthetic opioids mimic the body’s own endogenous opioids, meaning they can use those same receptors to send feel-good signals to the brain.
The problem is that “Although these drugs mimic brain chemicals, they don’t activate nerve cells in the same way as a natural neurotransmitter, and they lead to abnormal messages being transmitted through the network,” explains the National Alliance of Advocates for Buprenorphine Treatment (2008).
Unfortunately, the abnormal messages that non-endogenous opioids send are far more powerful than those your body can manufacture on its own, so normal pleasure-inducing activities just can’t compete. In a choice between the drug and a normal activity, the drug will always win.
The Hazards of Addiction
Opioids lower the perception of pain, as they trigger pleasurable chemicals to be released in the brain, thereby activating the reward system deep in the brain tissue. Our brains associate the action of taking an opioid with a pleasurable, rewarding event. The brain wants to continue to enjoy these pleasurable events and actions. This often leads to a subconscious craving for more drugs. Another way of putting it is that the brain has learned that using opioids is an enjoyable and positive experience that it should have as often as possible.
As the user continues to take opioids more regularly, the brain learns to tolerate them. Tolerance means that the person needs more of the drug to enjoy its effects. For example, you may need two pills per day at first to reduce pain. But if you continue to take them, you will need three or four pills or more to get the same effect. Over time, you will often need more of the opioid to get the identical effect. This is the reason that opioids are so dangerous, and efforts should and are being made to limit their use.
Opioid Tolerances
There is another factor at play too, however. The brain quickly grows accustomed to the levels of opioids it is fed. If you give it normally small doses of opioids from a daily workout, it feels good, and normal levels of opioids will work again. If you flood it with euphoria from heroin, however, the brain quickly adjusts to this “new normal,” and expects those levels every time. Thus, even if you do try a normal opioid-inducing activity such as exercise or sex, the results will be so much smaller that they may not feel pleasurable at all. It’s common, in fact, for addicts to express despondency over the fact that activities they used to enjoy bring them no pleasure anymore; only the drug matters.
The Crux of the Dependency
This is the crux of dependency: that your body cannot function “normally” without it. It craves it above all else – food, drink, sex, love, everything. Over time, with long periods away from the drug, the body can recover its ability to respond normally to stimulus, and such normal activities will once again become rewarding. However, this can take months and often years, and the brain never fully forgets the extreme rewards it used to feel in response to the high of opioids – which means relapse is a danger until the end of the former user’s life.
Therefore, prescribing opioids is inherently very dangerous and must done only when medically necessary. The initial reason for the prescription is usually sound (although it isn’t always) – to reduce pain and increase comfort – but the side effect of tweaking the brain’s reward center can pose a high degree of long-term risk. The hazards are all too real.
Opioid overprescription is even more dangerous because some addicts have discovered ways to alter the drugs to get instant highs. These adulterations are incredibly hazardous and addiction is commonplace.
Ways Opioids Are Abused
It is common for people to be prescribed OxyContin, Percocet, Percodan or Roxicet, all of which contain the opioid oxycodone. These drugs can be prescribed in tablet, capsule or liquid form, depending upon the nature of your pain and what the doctor prescribes. However, people who abuse opioids may grind the tablets into a powder, which can be snorted or injected. Snorting oxycodone greatly speeds up the effect of the drug on the nervous system. The result is a drug high that is similar to taking heroin.
OxyContin is a popular, extended release version of oxycodone. It is one of the most popular drugs to be abused. Available doses for the drug are from 10 mg to 160 mg. But when the timed-release coating is taken off, the drug can be crushed and snorted. Snorting OxyContin allows the drug to be absorbed quickly through the mucous membranes in the nose. It is this type of ingestion of opioids that has largely led to the epidemic of opioid dependence.
When the protective coating is removed from oxycodone and snorted, the effects can be very dangerous, including:
- Sudden decrease in blood pressure
- Slow or irregular breathing
- Nausea
- Seizures
- Cardiac arrest
Also, people who drink alcohol and snort oxycodone can have a great increase in the chance of a deadly overdose. Abuse of these adulterated drugs can lead to a vicious downward spiral into other forms of drug abuse.
Some Users Turn to Other Drugs
As people grow increasingly addicted, but can no longer get their fix through prescribed channels – or from friends and family – they are turning to worse channels, such as black market synthetic opioids, or even heroin. On the surface, this might appear to be a problem created by addicts who can’t control themselves. But the story is a little deeper.
Clearly, the pharmaceutical industry has a hand to play in the current crisis, as do medical professionals who hand out the drugs too freely. Many doctors not only prescribe opioids to manage pain from chronic conditions or traumatic injuries. They also add additional “as needed” opioids to the mix to take as flare-ups, called “breakout pains,” arise. This gives people a measure of control over their own prescriptions that some question – at what point does taking these medications go from necessary to recreational? In many cases, physicians can prescribe fewer pills at one time. However, it would be a gross overstatement to say that medical professionals, who in most cases merely want to see their patients find relief, are fully to blame.
But Some Patients Desperately Need Pain Relief
Then, of course, there are those who actually take opioids on a regular basis to manage chronic pain, or who take it when dealing with an acute trauma, such as an accident or surgery. There exists, and rightly so, a huge amount of concern about these people and their medical teams that without adequate pain medications, we will return to a pre-1990s state, where people experienced intolerable levels of pain and longer healing times because these drugs were so widely stigmatized.
A brief scan of quote collections on the subject will demonstrate the major concern expressed by people dependent on them for normal functioning. Consider this brief sampling from Goodreads (2017):
“Anyone who takes opioids on a regular basis will become dependent upon them, meaning they will have to taper off gradually to avoid withdrawal symptoms. But very few chronic pain patients exhibit the compulsive drug-seeking behaviors of someone who is addicted.” ~ Karen Lee Richards
“In the debate over opioid addiction, there’s one group we aren’t hearing from: chronic pain patients, many of whom need to use the drugs on a long-term basis.” ~ S. E. Smith
“[T]he media coverage of the ‘opiate epidemic’ as driven by pill pushing-doctors and by pain patients worries me a lot, and I think it is already being used to forward the idea that people in chronic pain should not have access to relief from their pain.” ~ Anit
Many other exhibit the same fears that because so many people are overdosing and dying, those who really need it will be unable to get it. Even those who have been on opioid pain medication for years as a palliative response to well-diagnosed chronic conditions have been experiencing longer wait times, the necessity for more frequent prescription refills in smaller amounts, and hassling from pharmacies. That’s good if the person being hassled is an addict who needs help. When it’s someone whose quality of life depends on the prescription, it’s not good at all.
Whatever the reason that the user has become hooked on opioids – either due to a legitimate prescription that spiraled out of control, or the drugs were stolen or bought on the street – reversing the addiction is paramount.
Reversing the Addiction
Opioid addiction is clearly a very serious problem. That is why some experts advocate for some non-traditional ways to fight addiction. They say that to get the opioid epidemic reversed, some outside the box thinking is required.
The US government and its agencies can be a major part of reversing the opioid addiction problem, according to a report in the Oct. 24/31, 2017 edition of the Journal of the American Medical Association (JAMA), if it takes these actions:
Improve Surveillance of Opioid Addiction
There are no current information systems that allow real time assessment of patterns, numbers and trends of new opioid addiction. This means that it is impossible at this time to track how the epidemic is progressing. Nor is it possible to identify the areas where opioid addiction is getting worse and intervene, and to learn lessons from areas where the problem is lessening.
Using systems such as the Prescription Drug Monitoring Program (PDMP) and other similar data systems to identify trends and patterns of new addiction, aggregate data might be used on a real time basis to pinpoint the factors that are associated with opioid addiction. New cases of opioid addiction might be going down, but deaths from heroin use could be going up due to the spread of fentanyl use. But it is impossible to know these things until incidence of opioid addiction is more effectively tracked.
Improve Reporting of and Response to Opioid-Caused Deaths and Overdoses
JAMA reports that real time data on drug overdoses from surveillance systems can allow faster response to patterns of changing opioid abuse across the US. More reliable data on the specific types of opioids that are involved in overdose fatalities would inform public health and law enforcement more effectively.
Also, improvements in the timeliness and quality of coroner and medical examiner work, including full access to PDMP data, could improve the timeliness and completeness of data. Further, improved training and more funding for medical examiners and coroners could allow more accurate identification of the drugs that are involved in overdoses.
Fatal and nonfatal drug overdoses that involved prescriptions need to trigger a report immediately to the healthcare professional of the patient. This will facilitate the proper medical response to the state medical board. People who survive the overdose also could be referred to treatment. This type of full feedback loop could encourage prescribing in a more cautious manner.
Promote More Cautious Prescribing for Acute Pain
It is understood that opioids are essential drugs for treating serious pain after surgery or serious injury. But they are prescribed too often for pain that may be treated with more conventional medications. For example, some dentists will prescribe opioids for molar extractions in adolescents. This type of prescription may be an excessive use of opioids.
When a prescription for opioids cannot be avoided, the dosage and duration should be as little as possible. It is important to remember, JAMA reports, that physiological dependence on opioids can occur in as little as a week. Patients who are taking a short prescription of opioids can experience substantial withdrawal symptoms. This can lead to worsening of pain after stopping the taking of the drug, which can lead to more use of the drugs.
A recent clinical study reported by JAMA found that 20% of patients who were prescribed opioids for 10 days became long term users. Another clinical study found that the number of pills given for acute pain after surgery could be reduced by at least half and that less than 1% of patients ever needed a refill.
The Center for Disease Control and Prevention recommends that when opioids are given for acute pain, three days or less is often enough, and more than seven days is rarely needed. FDA also should revise its opioid labels to be consistent with the recommendations by the CDC. Adding duration of use to labels for opioids would send a strong message to healthcare professionals and patients that the risk of addiction increases when use is more than three days.
Alter Labeling for Chronic Pain and Restrict Use for This Purpose
The risk of opioid addiction is greater than the benefits for chronic pain that stems from problems such as low back pain or fibromyalgia. However, patients who have chronic pain unrelated to cancer have been a highly prized market for drug manufacturers. This accounts for much of the increase in opioid use in the US during the last two decades. FDA should, JAMA states, narrow the on label indications and stop marketing of opioids for low back pain and other health problems where the risks outweigh the benefits.
This change could discourage healthcare professionals from starting chronic patients on opioids. But it would not prohibit them from continuing off label prescribing of the drugs for stable patients with a chronic pain problem.
Increase Health Insurance Coverage for Pain Management With Non-Opioids
While chronic pain is a serious problem for millions of people, opioids are more dangerous than many other types of pain management. Full reimbursement for non prescription pain relievers, such as acetaminophen or NSAIDs, would remove the financial disincentives for patients. Easier access to and no copays for physical therapy and other pain management without drugs could reduce the chance of opioid abuse.
Stop the Supply of Illegal Opioids
Just as with alcohol and tobacco, if heroin and synthetic opioids such as fentanyl are made more expensive and harder to get, their abuse is likely to decline. Also, the legal system can implement new programs, including drug treatment instead of prison time, and correctional facilities can offer treatment for drug addicted inmates, with linkage to drug treatment programs when they are released.
Expand Treatment Access
Many patients who would benefit from being treated with methadone or buprenorphine will only get it if it is a more attractive option and more accessible that prescription or illegal opioids. For example, opioid overdoses in France dropped nearly 80% six years after there was widespread prescription of buprenorphine. Access to these drugs could be expanded if the US government takes down regulatory barriers and requires healthcare plans to offer buprenorphine treatment.
Remove High-Dose Opioids from the US Market
Commonly prescribed versions of opioids are dangerous, and some experts say they should not be on the market. For instance, a patient who takes an 80 milligram tablet of oxycodone two times per day is consuming a dosage that is associated with a much higher risk of death. Only one pill at a time is taken, so people may not understand what a high dose this is. A single pill that is diverted from a prescription could lead to a deadly overdose.
Implement Harm Reduction for Current Drug Users
Access to clean drug syringes can prevent infectious disease spread, and having more access to Naloxone (mentioned in more detail below), can lead to a reduction of fatal overdoses. The US government should assist state and local partners in making Naloxone and clean drug syringes more widely available. Also, FDA should approve an over the counter version of Naloxone.
Other possible ways of reversing opioid addiction outside of government action include:
Medical Marijuana
Some people may resist the idea, but Dr. Mehmet Oz, best known on television as Dr. Oz, thinks that medical marijuana could actually serve as an exit drug to help people overcome opioid addiction.
During a recent appearance of Fox News, Dr. Oz defended the use of medical marijuana. “People think that it is a gateway drug to narcotics. It may [actually] be the exit drug to help us get out of the narcotic epidemic.” (High Times).
Oz further criticized how cannabis is scheduled by the US government; because it is considered a Schedule I narcotic, it is hard for researchers to understand its full possible benefits in the war on opioid addiction.
Naloxone
Naloxone is a common medication used to quickly reverse opioid overdoses. It is classified as an opioid antagonist. This means that it binds to opioid receptors, and can block and reverse the effects of most opioids. It is used to restore regular respiration to an overdosed person whose breathing is abnormal or even stopped due to an overdose of opioid pain medications or heroin.
Naloxone has been shown to be very successful in reversing opioid overdoses. It is actually on the WHO’s Essential Medicines list. This is a fast-acting, short-acting drug. It does the job fast and only stays in the addict’s system for up to 90 minutes.
Some maintain that giving addicts Naloxone encourages the addict to take more drugs. However, research available at DrugAbuse.com states that the drug does not encourage the person to engage in further substance abuse. Their cited research suggests that it decreases the use of opioids. When it is administered properly, naloxone blocks the effects of opioids and causes the drug addict to experience withdrawal symptoms.
Some other opponents of using Naloxone to treat drug addicts also state that the use of the drug prevents the addict from getting drug treatment. Research indicates that there is nothing to suggest that the drug discourages drug addicts from going into a rehab program. This is, advocates claim, the one drug that can save an overdosed addict from certain death and provide a chance to get professional help. A near-death experience from an opioid overdose often serves as a wake up call to get clean.
To summarize, opioid addiction is clearly very serious and leads to many negative consequences for millions of Americans. Getting the problem under control and reversing reverse addiction problems is possible if the above actions are taken. A big part of reversing the trend is to limit the quantities of opioid prescriptions written every year in the US. Below we provide information how this is being done.
Solving the Prescribing Problem

Solving the Opioid Epidemic first requires recognition that the problem exists. Fortunately, as noted at the beginning of this article, recognition is coming from the highest authorities in the US: The White House recently stated that the epidemic is a national emergency. This statement from the top of the federal government has brought a high level of exposure to this crisis. This is significant.
Now that the Opioid Epidemic has been recognized at a national level by the president and other major stakeholders, more can be done to fight the problem. A major way to reduce the problem is to more effectively deal with how opioid prescriptions are handled and prescribed across the US. There are many moving parts in the effort to reduce the number of opioid prescriptions.
By coordinating the implementation of those moving parts, we can develop innovative approaches that encourage the safe prescription and use of opioids, which can greatly reduce the risk of abuse. For example, government agencies at the federal level can direct more resources toward reducing the number of prescriptions written by doctors. Physicians can more carefully monitor to whom they are prescribing the drugs to ensure the person does not have a drug addiction problem.
Pharmacies can take action by limiting how many pills are in a prescription. Health insurers can determine which doctors are prescribing the most opioids and why. And drug manufacturers can change how the drugs are formulated to reduce chances of abuse.
Below is more information about the stakeholders and efforts involved to solve the prescribing problem.
Government Agencies Role
The following state and federal agencies are working diligently on support and response efforts to help curb this epidemic. Learn more about what each agency is doing today.
Centers for Disease Control
In 2017, the Centers for Disease Control and Prevention (CDC) awarded $12 million to 23 states to support effective responses to the opioid overdose epidemic (CDC, July 17, 2017). It was reported that the money will be used to increase prevention efforts and to more effectively track overdoses related to abuse of opioids. CDC reported that $7.5 million will go to 20 states to track and prevent nonfatal and fatal overdoses of opioids.
Federal Drug Administration
FDA has played a very active role in fighting the opioid epidemic, and this is continuing. FDA in 2017 has been changing how it regulates opioid painkillers. And it has been partnering with unusual allies to fight the epidemic, including health insurers and companies that manage prescription drug benefits.
State Governments
Some of the efforts states can make to reduce opioid prescription abuse are:
- Increase the use of drug monitoring programs with the use of real-time data reporting and integrating it with electronic health records
- Enhance access to medication-assisted treatments for people with opioid addiction
- Better use data to identify and address prescribing defined as high risk
All of these efforts by major stakeholders have made a significant dent in the problem of opioid addiction. But much work remains. You in your individual community also play a key role.
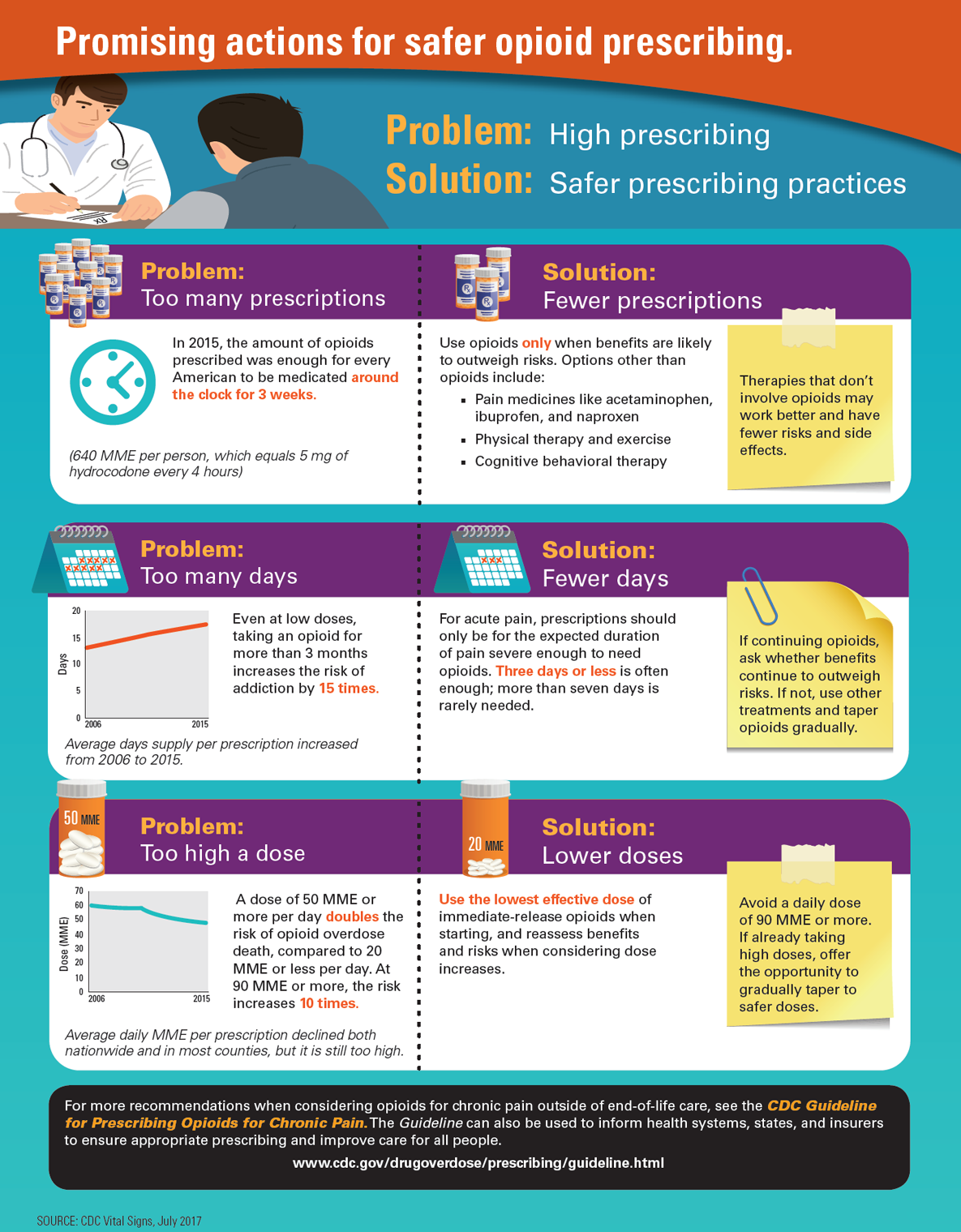
This graphic from the CDC shows other recommendations for healthcare providers in a problem vs solution scenario:
Below is more information about what each major stakeholder can and is doing including Doctors & Physicians, Pharmacies, Manufacturers & Distributors, Health Insurers and others.
Doctors & Physicians Role
One of the innovative ways that physicians are fighting the opioid epidemic is to use what is called the prescription monitoring program, or PMP. This program tracks all opioid prescriptions that are written throughout the country. Doctors hope to use PMP to reduce the estimated 13% of opioid prescriptions that are sought by patients with the intent misuse the drugs.
The PMP can track many types of opioid prescriptions, such as Fentanyl, OxyContin and Vicodin.
One doctor in Texas noted in a recent interview that he uses the system in his practice almost every day. For example, a patient will come in whose story is inconsistent with his illness, or, the patient will request an opioid prescription directly. The doctor will look up the patient’s name in the database and get an extensive report about the patient’s drug history.
Most US states are participating in the PMP program. The program also requires that all pharmacies in the participating state report all dispensed controlled substances to that state’s prescription monitoring program no later than the next business day.
Pharmacies Role
Pharmacies have been taking other actions in recent months to combat opioid addiction. In 2017, CVS Health, one of the largest managers of pharmaceutical benefits in the US, announced that it would limit the dose and duration of some opioid prescriptions.
CVS Health stated that it would place limits on opioid prescriptions to a week or less for some patients with acute pain who have not previously been on an opioid. This is a major change, as many patients covered by CVS with acute pain have been receiving a 20 day or more prescription in the past.
CVS also is limiting patients with chronic pain to a maximum of 90 morphine milligram equivalents (MMEs). CVS noted that it is basing these new limits upon CDC recommendations published in 2016.
There are ways around the new rules; doctors can appeal the limits, and employers and insurers can opt out if they do not want the rules applied to their patients. Still, CVS Health maintains that its new opioid prescription rules will ‘reduce the amount of suffering that results from people being addicted to these medications.’
Manufacturers & Distributors Role
In the mid-2000s, public health officials and the manufacturers of opioids became aware that the drugs were sometimes being overprescribed and/or abused, leading to the opioid epidemic.
As a response, Purdue Pharma, the manufacturer of OxyContin, withdrew the formulation of the drug from the market. In August 2010, the company released a new form of the drug. It was designed to be more difficult to abuse. Several steps were taken to reformulate the drug to make it more difficult to adulterate. For example, the new drug was made to minimize the oxycodone available even after it was crushed. It also was made impossible to have a dissolved form of the drug to pass through a syringe for injection (Washington Post).
A study published in the journal Drugs and Alcohol Dependence used interviews from 190 people with a history of abusing OxyContin to assess how effective the new formulation was to discourage opioid abuse. During interviews, each person was asked to compare their level of opioid abuse before and after the reformulation.
Researchers determined that 33% of those in the study had attempted to abuse the new version of the drug in the 30 days before the study. On the other hand, 74% reported OxyContin abuse prior to the new drug being released. Also, 96% of study participants reported abusing any form of immediate-release oxycodone prior to the reformulation. (Journal of Addiction Medicine).
Rates for snorting and injecting the new form of OxyContin was also lower than the rates associated with the older version of the drug. Overall, participants attempted to abuse the new OxyContin on two out of 30 days. Abuse of the original OxyContin took place roughly 13 days per month.
Researchers also noted that abuse of the old drug among the study participants was much less common after the new formulation hit the market. They also noted that participants seldom switched from oxycodone abuse to heroin. Their conclusion was that for at least the patients in this limited study, the new formulation of OxyContin played a lesser role in the opioid abuse epidemic than the original version.
However, a working paper published by the RAND Corp. and the Wharton School found in 2017 that the reformulation of OxyContin may have been the chief driver of the increase in heroin overdose deaths. The paper claims that the reformulation was the largest driver of a change to heroin abuse. It claims that it accounted for as much as 80% of the 300% increase in heroin mortality since 2010. The paper further noted that while the OxyContin reformulation was successful in reducing abuse, each 1% reduction of OxyContin abuse led to 3.1 more heroin-related deaths per 100,000.
Health Insurers Role
The healthcare company Aetna has set a goal to reduce inappropriate opioid prescribing by 50% by 2022 (Aetna). The company is also trying to boost evidence-based approaches when it is treating people who suffer from chronic pain. Aetna’s goal is part of the organization’s bigger overall strategy to fight the opioid epidemic. According to its opioid strategy paper that was published in 2017, the company is using data analytics, clinical insights, and collaborations in the fight against opioid addiction.
The healthcare company Aetna has set a goal to reduce inappropriate opioid prescribing by 50% by 2022 (Aetna). It reports that for 2017, it estimates there will be 8,958,842 opioid prescriptions filled, which is a 10.85% decrease from 2016.
As part of these efforts, Aetna analyzed its insurance claims data to identify more than 1,000 doctors who were overprescribing opioids. These doctors were sent letters that warned them of their prescribing patterns. They also were provided with educational materials stressing the importance of only prescribing opioids when medically necessary. In 2017, Aetna continued this effort and sent more than 1,000 dentists and oral surgeons letters who were overprescribing the drugs.
Aetna also has enhanced its Controlled Substance Use Program. It identifies patients that might abuse or misuse opioids. The program also allows the company to contact prescribers and to contact the insurance holder to offer help.
The Experts Weigh In
Experts from various fields have weighed in for years about the opioid epidemic. By listening to them and relying on their expertise, we all can work together to save lives and to reduce the effects of this public health crisis. Below are recent insights from experts in the field who are leading the fight against opioid addiction.








Most Influential People on Twitter
Social media is packed with influential people but it’s a matter of finding who to follow which makes your quest for information worthwhile. The following list of twitter handles was determined by the number of likes and shares each has earned for posts containing #opioid related hashtags. To stay on top of the latest opioid epidemic news, we advise you follow a number of these top 35 influential people now.



































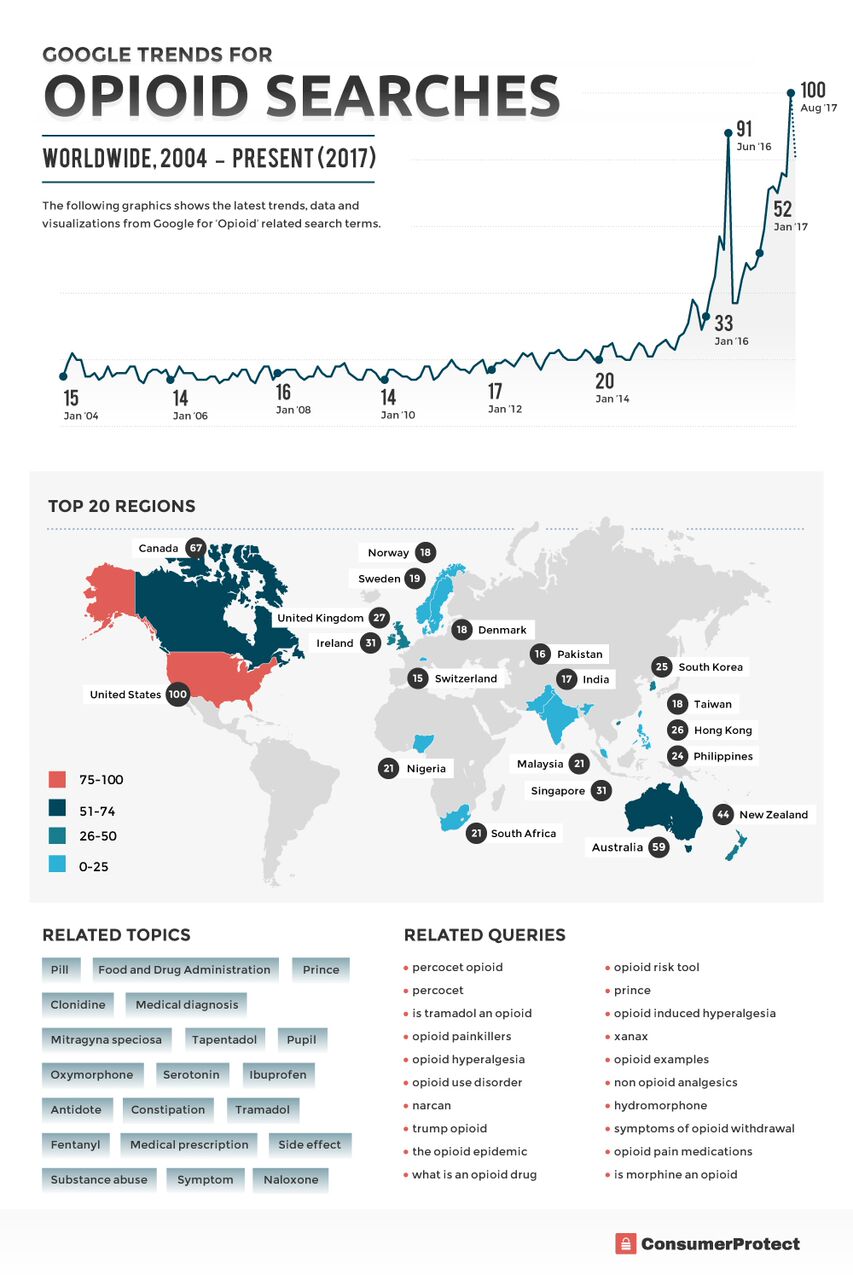
Worldwide Opioid Search Trends
See the latest trends, data and visualizations from Google. See how Opioid related searches have trended over time.
Helplines & Resources

The opioid epidemic is extremely serious and overcoming addiction is fraught with challenges. The problem that many drug addicts have is that they often think that they can stop abusing drugs without help. This is rarely the case.
Fortunately, there are ample state, local and national resources available to help people with their drug addiction problems. From treatment programs to support groups to medical help, you can get help for your drug addiction. Below are some of the resources available to help with opioid addiction. We also have included resources for experts in the field, as well as general drug addiction information for the public. Also included is an extensive list of helpful drug addiction-related blogs.
Please review and consult the following helplines and resources:
Websites and Helplines
- Drug Abuse Hotline: 1-877-413-6436. General drug help hotline.
- Covenant House Teen Hotline: 1-800-999-9999. For adolescents, teens and families. Help with any type of issue, including drugs and alcohol.
- National Institute on Drug Abuse: 1-800-662-4357. Hotline for preventing and treating drug abuse. 24/7 help to find a local drug rehab facility.
- Partnership at Drugfree.org: 1-855-378-04373. Not a hotline; intended to offer helpful information to parents about teen drug abuse.
- National Suicide Prevention Lifeline: 1-8900-273-8255. Hotline for both suicide and help for people with drug and alcohol addiction.
- Seeking Drug Abuse Treatment: What to Ask: A review of the critical questions to ask when seeking an effective drug treatment program.
- The Support Group Project: Online directory that assists American families to locate support to assist with a loved one’s drug addiction.
- Addictioncenter.com: Helpful resources for people with drug addictions and their loved ones.
- Substance Abuse Treatment Facility Locator: Use this tool to locate the best drug treatment programs; features a large national database of recovery centers.
- Celebrating Lost Loved Ones to the Opioid Epidemic: The rise in deaths due to prescription drugs and heroin is alarming. Often times society may have a perception of who this is. The fact is they are everyday people we love, everywhere. Click “Add Lost Loved One” or “Participate” to add loved one.
Public Education
- Shatterproof: A national nonprofit organization that is dedicated to ending drug dependency and addiction in American families.
- Easy to Read Drug Facts: Plain and simple language about drug facts; includes audios and videos from the National Institute on Drug Abuse.
- The Hungry Heart: A behind-the-scenes look at the frequently hidden world of prescription drug addiction.
Opioid Experts
- Helping Others Live Sober: Drug addiction resources for experts and professionals in the addiction medicine field. Provided by the Case Western Reserve University School of Medicine.
- Addiction Treatment Forum: Extensive coverage of substance abuse news that is of interest to experts in the field, as well as patients undergoing treatment.
- Stanton Peele: A psychologist who has pioneered new ideas in the field of addiction. The site includes some of his most widely read articles and books, such as Why Addiction Isn’t a Disease.
- Gabor Mate: Renowned drug addiction expert who calls for more compassionate approaches to addiction. Believes the source of addiction for most people lies in the childhood environment.
Addiction News and Trends
- Addiction Unscripted: Source for addiction recovery news, reviews of rehab centers and other resources.
- DrugAddictionSupport.org: News and current topics about drug addiction.
- AddictionBlog.org: Review of the latest trends in chemical addiction and about the newest discoveries in how addiction is treated.
- Rehabs.com: Covers drug rehabilitation news, as well as addiction treatment programs and how to sustain recovery over the long term.
Addiction Recovery
- Addictions Recovery Blog: Offers extensive discussions of addiction treatment, recovery and support services.
- Addiction Land: Designed to help addicts of all kinds. The blog features support resources, recovery experts and details about various paths of recovery.
- Smart Recovery Blog: Leading self-empowering addiction recovery support group; helps people to recover from drug addiction and other harmful behaviors.
- Kill the Heroin Epidemic Nationwide: Receive timely news about heroin and opiate addiction and recovery.
- Memoirs of an Addicted Brain: Understanding the many diverse aspects of drug addiction.
- The Hurt Healer: An inspirational blog by a woman who has been in recovery for several years.
- It’s Not Always Crystal Clear: Honest and insightful blog about a mother and woman’s journey through drug addiction and recovery.
- The Fix: A leading site for addiction and recovery, with a blog that has many expert voices about how to overcome drug addiction.
- Sober Julie: An unusual take on sobriety and addiction recovery; many ideas for food and non-alcoholic drinks, tips to stay sober and reflections on life.
- The Clearing: Informative articles about various types of addiction; how to stay sober; break addictions and self-healing programs.
- Sobernation.com: A national resource center for people who are trying to recover from drug addiction and alcohol addiction.
- Sober Long Time – Now What? A weekly blog that deals with the challenges and joys of living a drug-free life.
- Waking Up the Ghost: Touches on many aspects of living a life successfully in recovery.
Public Health
- The Healthcare Blog: Dense and content-rich, this blog gives a compendious 360-degree look at all things health care, ranging from legislation to payors to tech. A rich insiders resource.
- Health Wonk Review: A biweekly compendium of the best of the health policy blogs founded by Joe Padula and Matthew Holt.
- The New York Times: Well: This blog is designed for the public instead of health care providers; contains scientific, research-based content about various health problems.
- Susan Blumenthal: Huffington Post: Rear Admiral Susan Blumenthal, MD, provides blogs and articles about drug addiction and many healthcare problems afflicting the public.
- Health News Review: Health News Watchdog Blog: Dedicated to evaluating healthcare journalism, marketing, advertising, PR and more.
- Center for Disease Control and Prevention (CDC) Public Health Matters Blog: This blog provides helpful information for scientists and researchers, as well as the general public.
- Huffington Post Health News: Covers health issues that are geared toward members of the public.
- Healthcare Economist: Written by Dr. Jason Shafrin, founder, editor, and chief writer.
- HealthBlawg: Written by David Harlow, healthcare lawyer & consultant, with over thirty years of public and private sector experience.
Mental Health
- Therese Borhard: Blogs about emotional survival, depression and mental health.
- Amy Marlow: A blogger who blogs about surviving suicide of a loved one; her father committed suicide when she was 13.
- Bill White: A blog with an emphasis on depression, anxiety, stress, and bipolarity.
- Erin Schulthies: A blogger who has struggled with severe depression since she was a child.
- Deborah Serani: Practicing psychoanalyst who treats trauma and depression. She also has written several award-winning books on depression.
- Douglas Cootey: Blogs about overcoming ADHD and depression, with a lot of humor and attitude.
- Chipur: Operated by Bill White, founder, and producer of Chipur.
- TheMighty: They are creating a safe platform for their community members to tell their stories, connect with others and raise support for the causes they believe in.
- Rethink: Their goal is a better life for everyone affected by mental illness. See how they make a difference
- BeyondMeds.com: The site documents and shares many natural methods of self-care for finding and sustaining health in body, mind, and spirit.
- HealthyPlace.com: At HealthyPlace.com, you’ll find comprehensive, authoritative information on psychological disorders, psychiatric medications, and other mental health treatments.
- NatashaTracey.com: Natasha is considered a subject matter expert in bipolar disorder and her thoughts on it have been sought by the media and academics.
Rehab Centers
- 12 Keys Rehab: Addiction center in Florida that posts regularly about how to defeat drug addiction.
- ConsumerAffairs.com: Expert reviews and consumer reviews of many drug rehab facilities across the country.
- RecoveryConnection.com: Connects people who need treatment with the information and resources that they need to find the best treatment center.
- AddictionResource.com: Extensive selection of rehab center reviews; also has a local rehab locator, and a section about free and state-funded rehabs.
If you know of a great blog or resource we missed, please let us know and we’ll consider including it.
Recap & Conclusion

Clearly, the Opioid Epidemic in the United States is a deadly serious problem. Thousands of Americans continue to die from opioid overdoses every year, and at least 50% of those deaths are due to an opioid obtained through a prescription. Many victims do not die; instead, they become addicted to prescription and illegal opioids. Heroin, an illegal opioid, also has been responsible for a three-fold increase in deaths since 2010. These deaths and addiction problems associated with opioids have many detrimental economic and personal effects on American families. The effects on men, women, children and the economy are serious and growing worse.
While opioid abuse is a major public health problem in America, there is progress being made. Various preventative actions, treatments and effective responses to overdoses are helping. The US government and president have made public statements about the opioid problem being a serious crisis that must be confronted aggressively and with plenty of financial resources.
As this document has illustrated, much is being done and more can be done to fight this epidemic:
- Provide more oversight and caution in the prescription of opioid drugs
- Increase understanding of the opioid crisis through more effective public health reporting
- Engage with major opioid stakeholders – doctors, healthcare organizations, insurance companies, pharmaceutical companies, and state and local governments – to do their part to combat opioid addiction
- Offer better practices for managing pain
- Provide more information to the public about the hazards of opioid addiction and what to do for help
- Give more support for research on pain and addiction
- Further develop resources in our local communities to fight over prescription and abuse
This document also has shown the tremendous number of resources available to those who are struggling with opioid addiction. Never think that you can beat opioid addiction on your own because you can’t. But there are a huge number of resources available to you if you will only reach out and ask for help. With more aggressive education and public health efforts among all stakeholders, public support from American leaders, and expanding options for treatment, it is possible to prevail in the national Opioid Epidemic and save lives, while still providing essential pain relief to patients in desperate need of it.
Feel free to share the findings of our research on your website for any noncommercial purposes, but please link back to this page so our contributors earn credit for their work.





